
How To Get Rid Of Bloating This Bikini Season
We all want to look and feel our best. That’s why it is so annoying when bloating gets in the way — especially when it comes time to get in our swimsuits. There are several

We all want to look and feel our best. That’s why it is so annoying when bloating gets in the way — especially when it comes time to get in our swimsuits. There are several

Everyone’s health journey is different but each comes with its own set of challenges and triumphs. Katie Ozimek, beloved functional medicine health coach at Omnia, has her own story to tell… As a child, I

At Omnia Health, we see so many patients suffering from Irritable Bowel Syndrome (IBS). This has similar symptoms to Inflammatory Bowel Disease, but is not the same thing. When someone has been diagnosed with IBS,
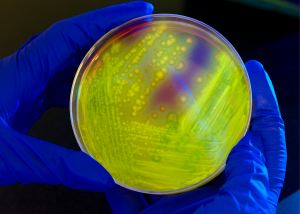
Picking up where we left off in our previous blog about gut health markers, there are two other important variables to test. For the sake of being proactive, efficient and accurate, we consistently test our

At Omnia Health, we believe in sharing our wealth of health knowledge. Helping others to feel their best is what motivates us every day. One of the ways we are able to fulfill that mission

At Omnia Health, we believe in trusting your instinct. When it comes to your overall well being, no one understands your body better than you. So if you feel like something is off, don’t let

(And what you can do about it) A lot of patients come to Omnia Health because they are struggling with irritable bowel syndrome (IBS). Some have lived with it for years. Their life is ruled

Have you ever gone to multiple doctors and done extensive lab testing only to be told, “Everything looks fine Your results are normal.” AND finally, after hours and hours of research, numerous doctor’s visits and

Is this you? You wake up to a beautiful Denver sunrise with a bloated and extended stomach. Immediately, you feel the urge to pass gas. As you dress for work, you spend time (you don’t

Omnia Health’s unique approach provides the best of both worlds: a traditional medicine background with a functional medicine approach.